Climate Change and the Effects on the Pulmonary System of Humans
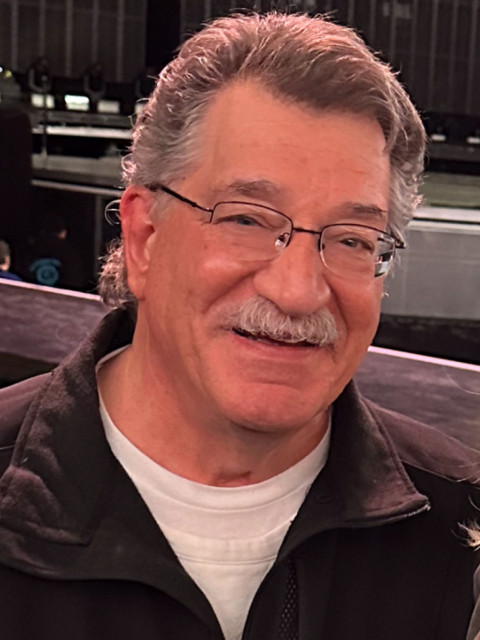
by Jack S. Tuber, DO, FACOI
Director of Clinical Research at Sun Valley Arthritis Center, LTD
June 13, 2024
Several different climate effects on the human pulmonary system are known and suspected to occur especially should we surpass 1.5C° of warming above the global average since 1850.
Pollution
The oil and gas sector caused air pollution in 2016 resulting in 410,000 asthma exacerbations, 2,200 new cases of childhood asthma and 7,500 excess deaths in the United States alone. The leading components of air pollution are nitrogen dioxide, ozone and particulate matter 2.5 (PM2.5). These pollutants are not only a consequence of the procurement and use of fossil fuels, but they also significantly contribute to climate change providing a “double-edged” sword contributing to pulmonary impacts and human health.
Wildfires
Being more frequent and of greater intensity because of global warming, wildfires are also contributing to new and exacerbating concurrent respiratory disease. The main pollutant is PM2.5, however carbon dioxide and other pollutants of combustion are contributing to worsening climate change in an apparent positive feedback loop.
Temperature
Global warming adds heat to the planet, thus adding the energy required to increase the frequency, intensity, and duration of extreme weather and climate events such as heat waves, floods, droughts and fires. A consequence of warmer temperatures reaching further north in latitude would be to allow vector-borne and non-vector-borne infectious diseases a foothold in environments in which they had not been previously seen. These new vectors may give rise to new, previously unseen respiratory diseases. Take for example higher surface temperatures allowing new soil conditions for fungal organisms to gain access. Weather conditions could then permit the spread of pathogenic organisms, such as Coccidioidomycosis, to infect populations who previously would not have been exposed. A higher incidence of fungal infection within humans would likely result in further numbers of those who would become symptomatic and to cases of dissemination, particularly in those who are immunocompromised.
Temperature increases are also projected to increase ozone pollution. Ozone’s effects on the human pulmonary system are well documented and include its own deleterious effects on the delicate cellular infrastructure of the lungs, as well as its chemical reactions with other molecules producing strong free radicals, causing further pulmonary damage. This, along with increasing particulates and likely allergic burden from increasing pollen, will further exacerbate respiratory diseases such as asthma and emphysema/chronic bronchitis, as well as cardiovascular diseases from particulates and ozone.
In addition, heat exposure is associated with an increase in mild to life-threatening respiratory-related diseases which includes COPD, asthma, and respiratory tract infections. The Wilderness Medical Society, the American College of Sports Medicine, and the National Association of Emergency Medical Service Physicians have all developed guidelines for diagnosis and treatment of heat-related conditions as a result.
Aeroallergens
According to computer modeling, a recent report (Nature Communications) indicates allergens are likely to increase up to 200% by the end of the century. Allergy “season” will be longer and more intense. This is much more troublesome than just annoying watery, itchy eyes and runny nose. These symptoms will accumulate giving rise to an increase in asthma exacerbations, respiratory infection, respiratory failure, hospitalizations, and even morbidity. In addition, this will translate to significantly higher health care costs, both in human and economic terms.
Flooding
The increase in warming also allows for the intensification of the hydrologic cycle, which causes more evaporation of ocean waters, giving rise to higher levels of atmospheric moisture. This in turn causes the so-called atmospheric rivers which we have been witnessing over the past several years. California has been in the forefront of this phenomenon recently and as stated above, vector populations will begin to change. Indeed, due to the amount of rain and consequential flooding, California is seeing an increase in Coccidioidomycosis infections. In addition, a recent report noted that children exposed to flooding during Hurricane Harvey had an increase in upper respiratory tract and allergic symptoms.
Human Nutrition and Immune System
As further changes in a once stable climate multiply, food scarcity will become more widespread. Together with the likelihood of less nutritious food, immunocompromised individuals will be more susceptible to host pathogens as well as invading organisms of the respiratory tract. In addition, as a greater percentage of the world’s population becomes immunocompromised, this phenomenon may exacerbate. Another consequence of climate change that we are already seeing is human migration from vulnerable areas such as deserts, wildfire prone areas, and coastal areas. Following Katrina, for instance, there has been a progressive migration of coastal residents to higher ground. At first, the initial movement was to escape the storm. But after years of being unable to rebuild and further severe storms, a permanent migration has taken place. The breakdown in social bonds and health care networks will no doubt have a deleterious effect on the care and ultimate outcome of those with respiratory diseases as well as diseases of other systems.
As can be seen by this short discourse, the severity of climate change on the pulmonary system of humans is multifactorial. Efforts to curtail the rise of carbon dioxide and other greenhouse gases are of the utmost importance.
References:
Air Pollution and Health Impacts of oil and gas production in the United
States, Bounocore, Jonathin J, et al 2023 Environ. Res.: Health 1 021006.
The Imperative for Climate Action to Protect Health. Haines, Andy and Ebi, Kristie, NEJM, 2019; 380:263-73.
Treatment and Prevention of Heat-Related Illness, Sorenson, C and Hess, J; NEJM, DOI: 10.1056/NEJMcp2210623.
Coccidioidomycosis and Histoplasmosis in Immunocompromised Persons, Galgiani, J, M.D. and Kauffman, C. A., M.D., NEJM, 2024;390:536-46.
Climate Change and Vectorborne Diseases, Thompson, Madeline C., and Stanberry, Lawrence R, NEJM 2022;387:1969-78.
https://www.nature.com/articles/s41467-022-28764-0
Climate Change, Fossil-Fuel Pollution, and Children’s Health, Perera, F., Dr. P.H., and Nadeau, K. M.D., Ph.D., NEJM, 2022;386:2303-14
Note: The views expressed in this article are the author’s own and do not necessarily represent the views of ACOI.

