Body, Mind, Spirit – Similar Training with a Touch of Distinctiveness
The philosophy of osteopathic medicine was developed in 1874 by Andrew Taylor Still, MD. Following the loss of three of his children to spinal meningitis, Dr. Still dedicated his life to studying the human body to find a better way to treat disease. Following research and clinical observations, he found that the body contained all the elements needed to maintain health, and that through the use of manual techniques (osteopathic manipulative medicine (OMM)), the body could be encouraged to heal itself by treating the whole patient and not just the disease.
The first osteopathic medical school opened in 1892 in Kirksville, MO. Today, osteopathic physicians are a growing segment of the physician community. There are 38 colleges of osteopathic medicine located at 58 main and branch campuses in 33 states. As a result, there are currently more than 33,800 osteopathic medical students. Osteopathic medical students now represent nearly a quarter of all medical students in the United States. With nearly 135,000 osteopathic physicians, DOs account for nearly 11 percent of the entire US physician workforce. Today, DOs are licensed to practice the full scope of medicine in all 50 states, in all specialties from internal medicine to obstetrics, surgery, aerospace medicine and more.
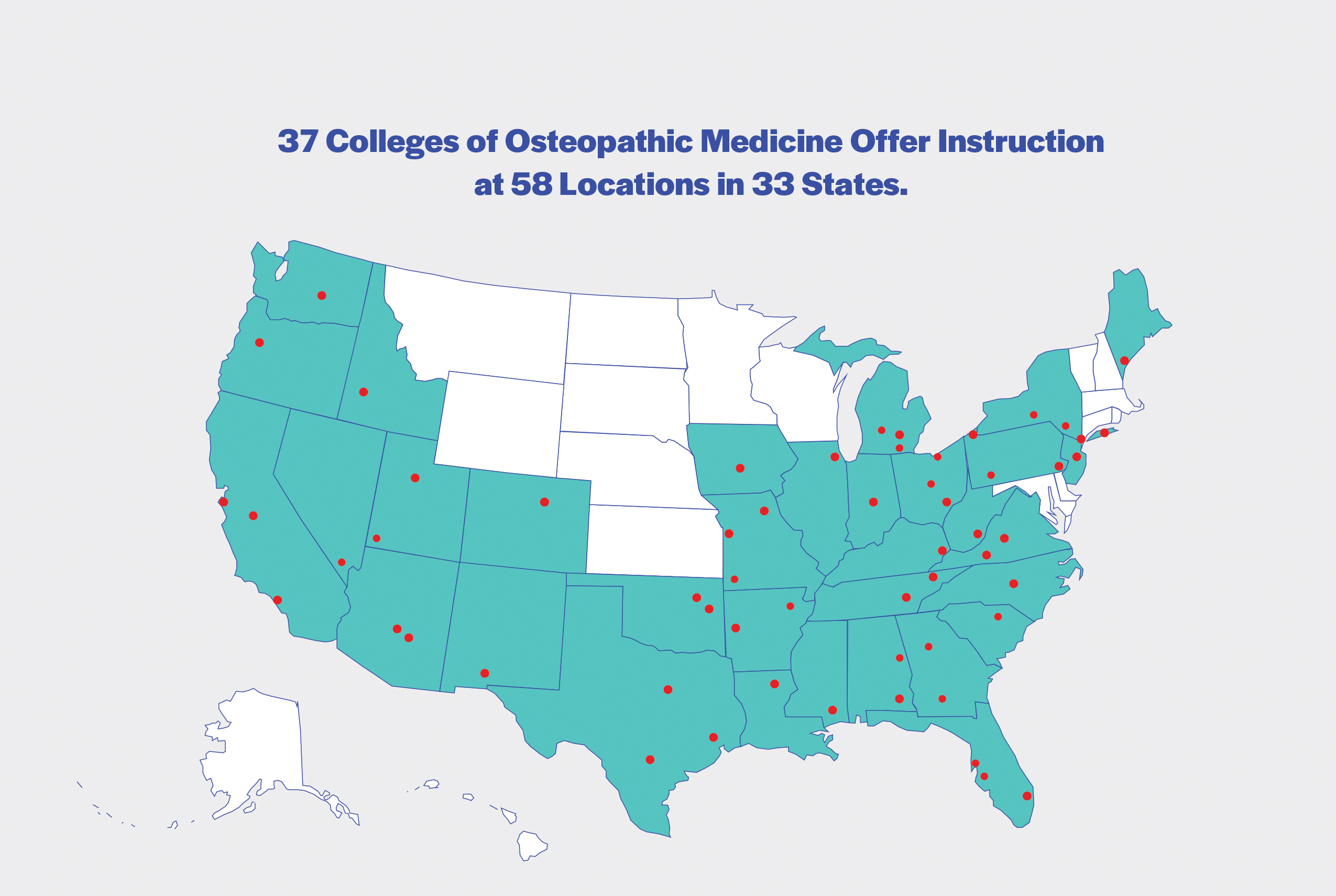
Source: AACOM
Why is Osteopathic Medicine Growing in Popularity?
From day one, osteopathic medical students are trained to look at the whole patient as more than just a collection of organ systems and body parts that become injured or diseased. Students learn to integrate the most modern science with OMM. It is this foundation of training, and approach to patient care that allows osteopathic physicians to provide compassionate whole-person care. At their core, osteopathic physicians are trained to listen to patients and work with them to treat them as a whole person and not just a symptom.

Source: AACOM. Click here to view full size.
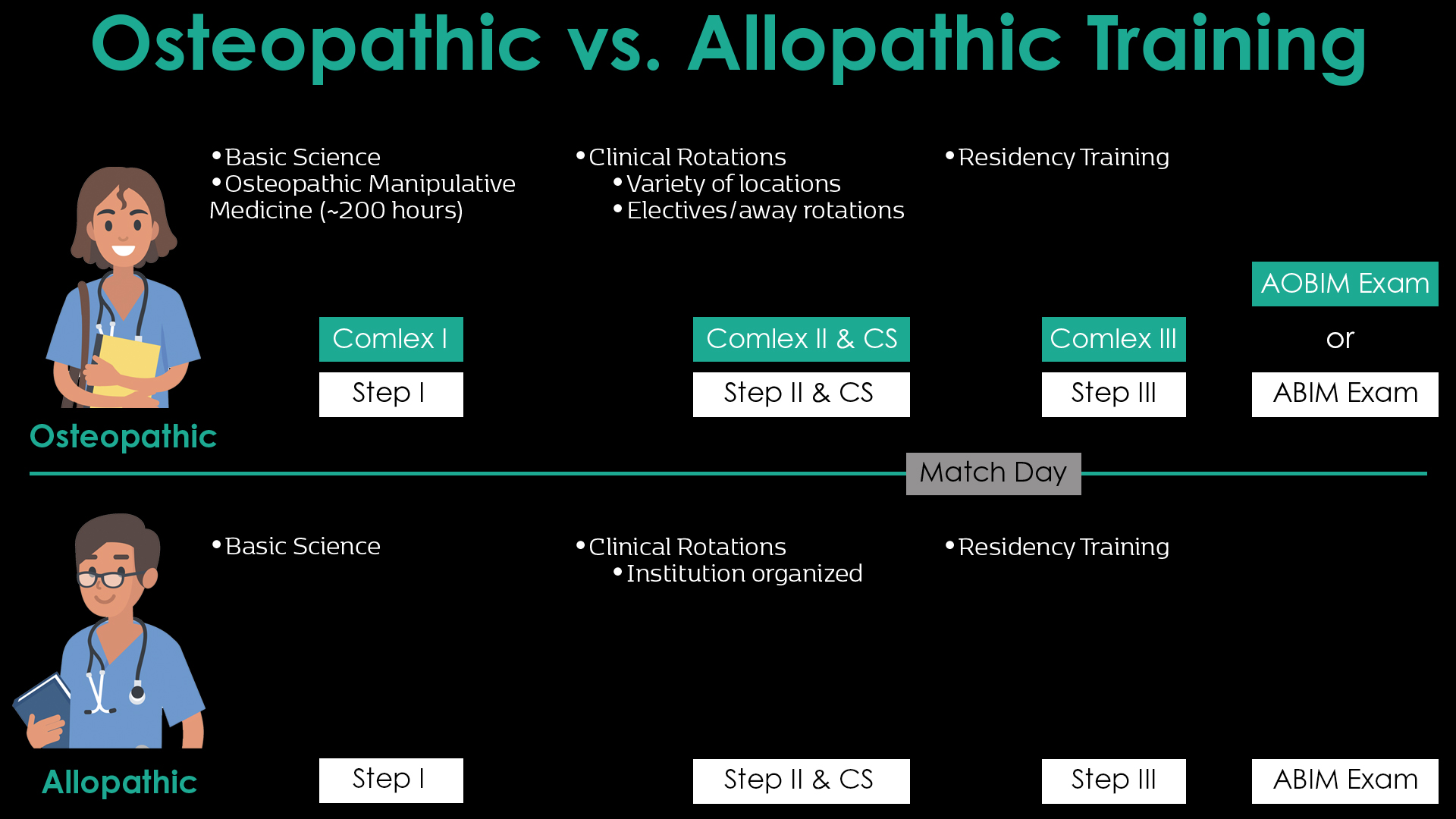
Similar Paths Lead to Becoming a Great Physician with Unique Learning and Experiences
The pathway to become a fully licensed physician, whether a graduate of an osteopathic or allopathic medical school is nearly identical in the core curricular activities. How is osteopathic medicine different? The primary difference is that an osteopathic medical student, in addition to the basic sciences, will study more than 200 hours of OMM during the four years of medical school. This includes hands on training that starts immediately after medical school matriculation. In addition, rotations for osteopathic medical students may occur in a variety of settings instead of at large academic institutions as is more common for many allopathic students. As a result, osteopathic students may benefit from a more diversified training experience and be able to apply this to future training and patient encounters.
Single Accreditation System Allows for Uniform Training Standards
In July 2015, a newly reimagined accreditation system for graduate medical education began to take shape when the American Osteopathic Association (AOA), American Association of Colleges of Osteopathic Medicine (AACOM), and the Accreditation Council for Graduate Medical Education (ACGME) began to create and transition to a single accreditation system for graduate medical education. As a result of the process that culminated with the full transition to the single accreditation system in June 2020, there is now a uniformed, consistent training process that allows for consistent evaluation and a uniform method to train the future physician workforce. The Single Accreditation for Graduate Medical Education system streamlined the training process and allows program directors the opportunity to compare trainees to one standard of post-doctoral training regardless of whether they graduated from an osteopathic or allopathic school.
Osteopathic Recognition Provides a Home For OMM
How is osteopathic medicine different in recognition? As part of the effort to move to a single accreditation system, and in recognition of the value OMM provides to patient care, the ACGME established a pathway for training programs to achieve Osteopathic Recognition. This designation is conferred by the ACGME’s Osteopathic Principles Committee upon ACGME-accredited programs that demonstrate, through a formal application process, the commitment to teaching and assessing Osteopathic Principles and Practice (OPP) at the graduate medical education level. This designation is in addition to the ACGME’s Common Program Requirements, which must be achieved by all training programs.
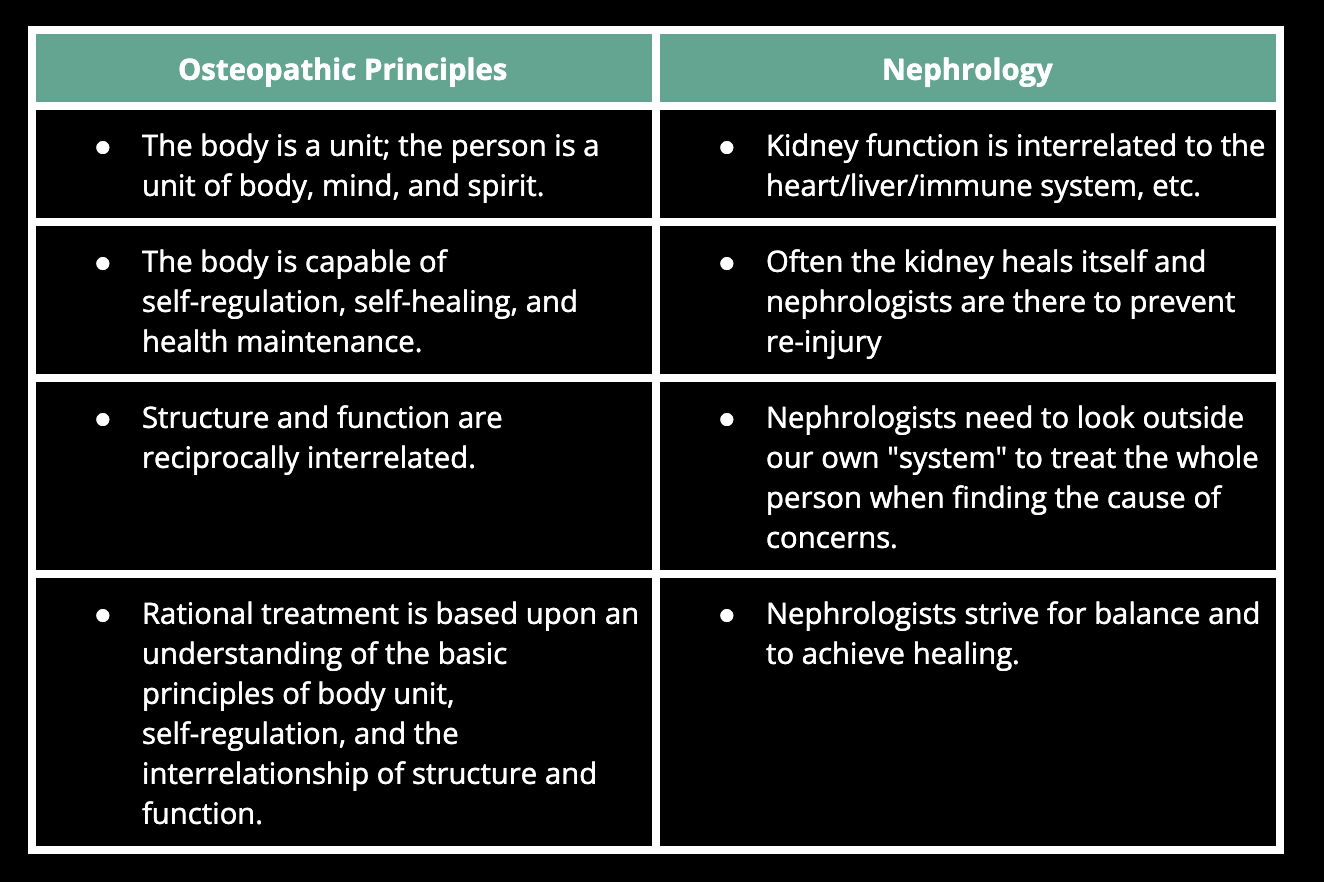
Nephrology: A Case Study
The tenants of osteopathic medicine make nephrology and osteopathic medicine a natural fit. While candidates for nephrology fellowship programs historically came from large academic institutions, the number of osteopathic internists, many of whom have traditionally trained in community-based hospitals, is on the rise. Osteopathic physicians have traditionally been drawn to primary care careers because it aligns well with the unique osteopathic principles. Nephrology offers a similar avenue to continue to practice these principles. The kidney is interrelated to many other systems in the body, it has the capability of self-healing and nephrologists often look toward systems outside the kidney to find answers. In addition, it is not surprising to hear that a nephrologist might be compelled to perform OMM to allow for the removal of NSAIDs to prevent harm to the kidney and allow for a discussion to explore other options for pain control. The additional OMM training coupled with osteopathic principles results in a more eclectic candidate that offers a greater diversity to any training program. As such, patient care is enhanced through the benefit of a broadened view of patient care.
Additional Resources:

