Vaccine Hesitancy and the Risks Posed by the Olympics
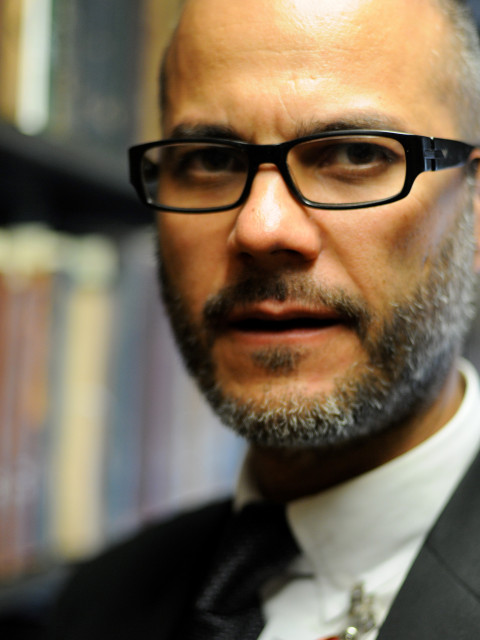
by MarkAlain Déry, DO, MPH, FACOI
Infectious Disease Specialist
August 4, 2021
As we’ve discussed many times during this blog in the last 16 months, the COVID-19 pandemic has universally surfaced inequities in healthcare. A study from researchers at the University of Minnesota and Hennepin Healthcare Research Institute (HHRI) was recently published in the JAMA Network Open. It is one of the first studies to examine testing for COVID-19 and how different socio-demographic groups used telehealth, outpatient clinic care, emergency department and inpatient care to test for SARS-CoV-2. For those of you who may not know, the JAMA Network Open is an international, peer-reviewed, open access, general medical journal that publishes research on clinical care, innovation in health care, health policy, and global health across all health disciplines and countries for clinicians, investigators, and policy makers.
The study revealed that:
- Patients who initiated COVID-19 testing through telehealth were disproportionately white and English-speaking. In contrast, patients who initiated testing through the emergency department were disproportionately Black, Native American, non-English-speaking and had one or more pre-existing conditions.
- Also, interestingly, testing that was initiated through telehealth and outpatient encounters was associated with lower rates of subsequent inpatient and intensive care unit care than testing initiated in more care-intensive settings, such as emergency departments.
So the natural question is why? The study pointed to structural root causes which included delays in seeking care, barriers to timely access to testing, putting off seeking care, difficulty in accessing telehealth and the higher rate of pre-existing conditions that require higher levels of care.
For many of us providers, we have seen the results of when communities of color delay care. Often it is delayed due to fear of how they will be treated and is linked to a history of racist events in medicine including the Tuskegee syphilis experiments that caused endless suffering for generations of Black Americans.
We saw that play out back a few months ago when the CDC released data that showed that Black Americans, had the lowest vaccination rates of any ethnic group, and a Kaiser Family Foundation poll at that time found about 35% of Black Americans said they would not get the vaccine due to concerns about trust, safety, and the newness of the vaccines.
Recently a story came out that has brought to light just how dangerous vaccine hesitancy is. Martin and Trina Daniel, ages 53 and 49 who both died on July 6 of COVID-19, and married 22 years, decided not to get the COVID-19 vaccine because of their mistrust in medicine based on the Tuskegee syphilis study. The study was conducted at the Alabama college where Martin ironically graduated from making this decision for he and his wife much more personal. That grave mistrust led to a fatal outcome and cost both of them their lives. As you may know, Alabama has the lowest percentage of fully vaccinated people. Mississippi, Arkansas, and my home state, Louisiana, also have less than 36 percent of residents fully vaccinated.
This is just one story of many of how distrust in medicine and the inequity in care continue to hurt communities of color and why I am so happy that the American Medical Association has released an 86-page “Organizational Strategic Plan to Embed Racial Justice and Advance Health Equity.” The AMA’s Health Equity Task Forces describes the paper as a roadmap “to embed racial justice and advance health equity for years to come.” The report is getting a lot of attention as more physicians now more than ever are speaking up about racial injustice.
Physician organizations are hearing more from members about combatting systemic racism. Not surprisingly, young people – students and residents -- have been leading the charge. Some will argue that physician associations are perhaps not the strongest way to lead transformational action on racial health equity. However, physicians, like myself who are seeking racial equity can enlist physician associations to help raise awareness.
For the ACOI the Committee on Health Equity and Inclusion in Medicine works to address issues related to underserved minority populations in continuing medical education and graduate medical education programs as well as to discuss areas in which the College may wish to create policy statements and provide advocacy regarding health equity and inclusion in medicine and to improve diversity in the pool of individuals recruited to careers in internal medicine. I hope that doing things like this video blog helps to disseminate important information regarding the impact of cultural differences on health care provision and outcomes.
We often discuss public health in the context of the United States, but as the 2020 Olympics move forward right now in 2021 in Tokyo, we are seeing a public health dilemma that is bound to impact every country on the planet. That dilemma started with the decision to move forward with the Olympic Games. Albeit these Olympics are without an audience at most events, but nevertheless, my concern has been the potential for these games to result in a superspreading event.
First, look at the fact that less than 10% of Japan’s population is fully vaccinated. Despite that this is happening during a historic pandemic, it is expected to be the most profitable yet for US TV stations in regard to advertising. In fact, NBC Universal sold 90% of its advertising inventory by March 2020 and hit a record of $1.25 billion, beating out the Rio Olympics in 2016 which recorded a $250 million profit.
Few of us realized that the Tokyo Medical Practitioners Association wrote an open letter in May to Japan’s Prime Minister recommending the games be canceled. They cited health concerns of course, fearing a COVID-19 outbreak associated with the event and as a result what that could mean as far as the disproportionate burden that would place on the country’s health system. Additionally, a survey reported that 83% of the Japanese population wanted the Olympics called off. While organizers required visiting athletes to follow a three-day quarantine upon arrival, many are saying that requirement felt unenforced and that there were crowds mingling at breakfast buffets. In addition, the health monitor app that was required, has failed to work.
The people really at risk here are the Japanese people with a full 90% of them unvaccinated. The rollout of the vaccine in Japan has been abysmal and those who have had a first shot have had their second shot appointment cancelled due to lack of supply. Of course, the highly transmissible Delta variant is increasing the risk and is accounting for at least 30% of the cases in Japan.
As of July 29, the new 7-day average of COVID cases in Japan rose from 1,589 on July 2 to 6,657 on July 29 breaking records both in the Olympic Village and throughout the city of Tokyo. The total number of infections within the Village is 193 with 24 more cases being reported July 29. Citywide, new cases across Tokyo, reached a record high of 3,865 on Thursday — the third straight day the city broke case records. Yet the International Olympic Committee has come out publicly to say that it is “highly unlikely the Games are a source of the infections.”
Stay on the lookout for out for these updates. Together with the ACOI we will help you have the latest information to help you respond to your patients. Please feel free to reach out to me at madery@mac.com. Please stay safe.
Sources:
- Study: Racial/ethnic and language inequities in ways patients obtain COVID-19 testing (medicalxpress.com)
- Vaccine Hesitancy in Communities of Color Eases -- A Bit (webmd.com)
- Black couple who refused vaccine because of notorious US government program die of COVID-19 | TheHill
- https://www.healthaffairs.org/doi/10.1377/hblog20210713.51887
- Are the Tokyo Olympics Safe? Locals Fear Public Health Crisis (verywellhealth.com)
- New COVID-19 cases surge in Olympic Village, across Tokyo (nypost.com)

